
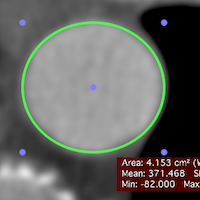
The greater the number of hydrogen nuclei experiencing fluctuations at the Larmor frequency, the shorter the T 1 relaxation time and the brighter the signal. For effective T 1 relaxation, the oscillations in magnetic field have to occur at a specific frequency called the Larmor frequency. As each hydrogen nucleus has magnetic properties, the rotational and tumbling movements of water molecules themselves act as the main source of magnetic field fluctuations. T 1 relaxation is a consequence of fluctuations in the magnetic field experienced by individual hydrogen nuclei, which in the body are predominantly bound within water molecules. (b) Matched post-contrast 10, 40, 70, 100, 130, 160, 190 and 220 s (1–8, respectively) images demonstrating the linear ROI on successive acquisitions (length 4.4 cm for each ROI, signal intensity values of 116, 179, 188, 181,192, 151, 156 and 134 for ROIs 1 to 8, respectively). Region of interest (ROI) placement was performed using OsiriX ( (a) Pre-contrast coronal T 1 weighted fat-saturated three-dimensional fast low-angle shot examination image of the ascending colon with a linear mural ROI (length 4.4 cm, signal intensity 109). In order to maintain the ROI within the colonic wall between successive acquisitions, the shape of the linear ROI was altered (with the length ☐.01 cm and anatomical position kept constant) to account for any colonic deformations. To guide ROI placement, the observers first reviewed the whole MR contrast-enhanced data set and chose those parts of the bowel wall reliably identifiable throughout the time series.
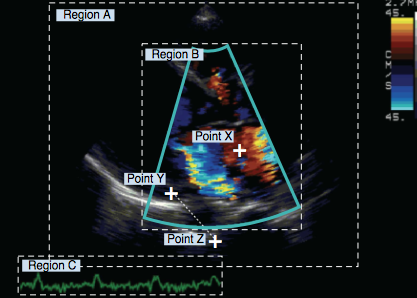
These segments were chosen as representative of the known differing vascular supply and functional properties of the colon over its length. Region of interest (ROI) analysis was performed on 3D FLASH MR images using the open-source OsiriX medical imaging platform ( Single freehand linear ROIs (mean size 5.4 cm range 2.3–9.8 cm) were located in the colonic wall of the ascending colon, descending colon and the lower rectum by a radiologist (SP) and gastroenterologist (RH) in consensus ( Figure 1). The purpose of this short communication is to present and discuss the quantitative MRI changes that occur following enhancement of endoscopically proven normal colon and to assess intersegmental differences.
In 15 normal volunteers, Ajaj et al have shown that at a single time point post contrast (75 s), relative enhancement differs according to colonic segment (being highest in the rectum and sigmoid, and lowest in the right colon and descending).Ĭlearly intersegmental differences of normal colonic enhancement will influence the interpretation of MRI in inflammatory bowel disease, in particular when assessing potentially inflamed bowel.
Colonic function also differs with proximal colon providing much of the water absorptive capability of the colon. Anatomical differences exist in segmental blood supply the right colon is supplied via the superior mesenteric artery, the left predominantly by the inferior mesenteric artery and the lower rectum via the iliac vessels. There are good reasons why enhancement may differ among bowel segments. non-inflamed) colon has received little attention. However, the baseline post-contrast enhancement of normal ( i.e. The reasons for this variability probably include differences in studied patient cohorts, applied standards of reference for disease activity (histological, biochemical, endoscopic or clinical) and methods of enhancement measurement (simple relative change in signal intensity at one time point, or more complex quantitative dynamic contrast enhancement techniques). Absolute post-gadolinium enhancement remains more controversial, with some workers finding high correlation, while others have found no relationship.
Various MRI parameters have been shown to correlate with disease activity, notably bowel wall thickness, T 2 signal and contrast enhancement pattern. distension of the colon usually via water enema). When applied to the colon, most workers have used the technique of MR colonography (MRC, i.e. MRI has shown considerable promise in quantifying inflammatory activity in Crohn's disease and ulcerative colitis.


 0 kommentar(er)
0 kommentar(er)
